Cholesterol constitutes a component within the clinical domains section of the Quality and Outcomes Framework (QOF).
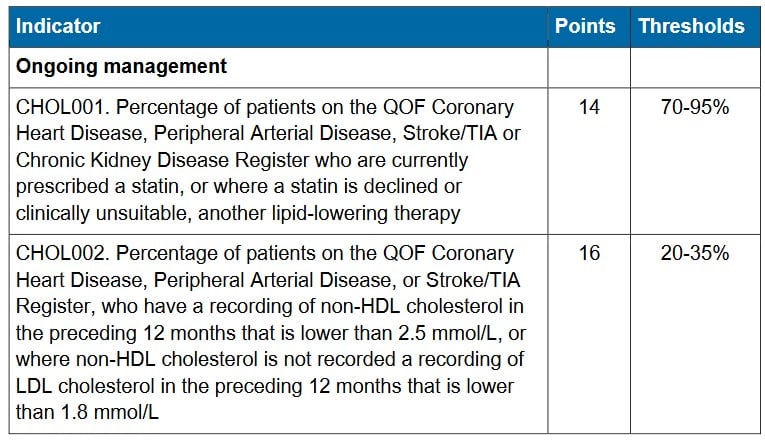
There exist two QOF indicators concerning Cholesterol:
- CHOL001 – This indicator encompasses patients listed in the QOF registers for Coronary Heart Disease (CHD), Peripheral Arterial Disease (PAD), Stroke/Transient Ischemic Attack (TIA), or Chronic Kidney Disease (CKD). It pertains to individuals who, during the last six months of the fiscal year, receive a prescription for a statin. Alternatively, if a statin is declined or deemed clinically unsuitable, another form of lipid-lowering therapy is prescribed. Patients aged 17 years or older, who are on any of these registers and concurrently diagnosed with diabetes, are excluded from this particular indicator.Personalized care adjustments (PCA) come into effect when patients meet certain criteria and have been properly coded with any of the following situations:
- The patient possesses a palliative care code on their medical record dated on or after April 1, 2008.
- They decline or are clinically unsuitable for both statin treatment and all available alternative lipid-lowering therapies within the current fiscal year.
- The patient’s medical record indicates they are on the maximum tolerated cholesterol-lowering treatment within this fiscal year.
- The patient’s medical record indicates an adverse reaction to lipid-lowering therapy or a code indicating that lipid-lowering therapy is not indicated, contraindicated, or declined within this fiscal year.
- Patients newly registered at the medical practice within the final three months of the fiscal year.
- CHOL002 – This indicator encompasses patients listed in the QOF registers for Coronary Heart Disease (CHD), Peripheral Arterial Disease (PAD), or Stroke/Transient Ischemic Attack (TIA). It applies to patients who have a recorded value of non-HDL cholesterol lower than 2.5 mmol/L within this fiscal year. Alternatively, if non-HDL cholesterol is not recorded, the indicator applies to patients with a recorded value of LDL cholesterol lower than 1.8 mmol/L within this fiscal year.Personalised Care Adjustments applies in situations where the patient either declines a cholesterol blood test within this fiscal year or has registered within the last nine months of the fiscal year.Personalised Care Adjustments refers to specific circumstances or criteria under which adjustments or exceptions are made to the requirements or conditions of the QOF indicators related to cholesterol management. These personalized care adjustments take into consideration various factors that might impact a patient’s eligibility or treatment plan, allowing for a more tailored approach to their care. The purpose of PCA is to ensure that patients’ individual needs and situations are considered when assessing their compliance with the QOF indicators and when determining the appropriate treatment or interventions for them.
CHOL001 – This indicator assesses the percentage of patients registered in the QOF for conditions like Coronary Heart Disease (CHD), Peripheral Arterial Disease (PAD), Stroke/Transient Ischemic Attack (TIA), or Chronic Kidney Disease (CKD) who are currently prescribed a statin. In cases where a statin is declined or not clinically suitable, another lipid-lowering therapy is considered. The achievement of this indicator carries a total of 14 points, with the requirement that 95% of patients on the CHD, PAD, stroke, and CKD registers receive statin treatment. This indicator amalgamates what used to be separate assessments within each of these domains into one comprehensive measure.
However, patients aged 17 and above with diabetes have a distinct indicator for statin prescription and are excluded from this new combined indicator, even if they have concurrent CHD, PAD, or stroke conditions.
Exceptions to this indicator include patients on the palliative care register. Given the substantial overlap between cardiovascular disease and diabetes, the number of excluded patients might be considerable.
Personalised care adjustments (PCA) may apply to patients who have declined a statin treatment. Regarding adverse reactions, the majority of patients will be prescribed a statin. Additionally, patients receiving bempedoic acid, ezetimibe, icosapent ethyl, inclisiran, or a PCSK9 inhibitor will be included in the indicator only if they have a documented adverse reaction to a statin. Notably, recording an adverse reaction or allergy to a statin will not exempt a patient from the indicator. Exceptions may also be granted if patients have codes indicating informed dissent or an adverse reaction to lipid-lowering therapy in general.
The standard prescription timelines apply, necessitating issuance in the latter half of the QOF year. Prescriptions spanning six months or more may not be captured by this indicator.
While patients with cardiovascular disease typically receive statin prescriptions, the number of chronic kidney disease patients prescribed statins might be lower. It could be advantageous to focus efforts on this subgroup at the beginning of the year.
For patients intolerant to statins, there is now greater emphasis on alternative medications. Patients who were previously exception reported might benefit from assessing the suitability of alternative cholesterol-lowering medications.
CHOL002 – This indicator gauges the percentage of patients registered in the QOF for conditions like Coronary Heart Disease (CHD), Peripheral Arterial Disease (PAD), or Stroke/Transient Ischemic Attack (TIA) who have a recorded non-HDL cholesterol level below 2.5 mmol/L within the preceding 12 months. Alternatively, if non-HDL cholesterol is not recorded, the indicator applies to patients with a recorded LDL cholesterol level below 1.8 mmol/L within the same timeframe.
There are distinct differences in this indicator. First, it excludes patients with chronic kidney disease. Second, it includes patients with diabetes or on the palliative care register, provided they are also on the CHD, PAD, or stroke registers. Consequently, the patient population assessed by this indicator significantly differs from CHOL001.
Presently, there are limited exception reports available for this indicator. Patients are excepted only if they decline a cholesterol test or register with the practice after July in the QOF year, with a specific code indicating a declined test triggering this exception.
As of the current business rules for the 2023/2024 period, there are no exception reports for treatment allergies, informed dissent, or being on the maximum tolerated treatment dose.
The indicator’s criteria remain consistent, with non-HDL cholesterol being required to be below 2.5 mmol/L. If non-HDL data isn’t available, LDL cholesterol should be less than 1.8 mmol/L. Non-HDL takes precedence over LDL measurements, even if subsequent LDL data is available. This prioritization is particularly significant in cases of changes in local lab reporting or patient movement between practices.
This indicator carries a total of 16 points, with low thresholds for achievement, starting at 20% and reaching the full 16 points for 35% attainment.
Given that this indicator uses codes not previously featured in the QOF, it’s crucial to ensure their recognition. These codes can be derived from lab tests, point-of-care patient tests, or transcribed from hospital letters. Maintaining up-to-date templates for manual entry is essential.
Identifying patients with elevated values, adjusting medication, and retesting demands time. Initiating this process early on enhances the likelihood of achieving high scores in this indicator. The cholesterol indicators together offer a total of 30 points.